PCOS and endometriosis: what this means for fertility
Being diagnosed with Polycystic Ovary Syndrome (PCOS), endometriosis, or both, can bring a lot of questions, especially if you’re thinking about starting a family now or in the future. While both conditions can impact fertility in different ways, they don’t mean pregnancy is out of reach.
In this article, Dr Apostolos Tsironis explore how each condition affects the reproductive system, what it means if you have both, and the many supportive treatment options available to help you on your journey to parenthood.
What are PCOS and endometriosis?
Although very different conditions, PCOS and Endometriosis are both common causes of fertility challenges, and it’s not unusual to feel confused or overwhelmed after receiving a diagnosis.
Polycystic ovary syndrome
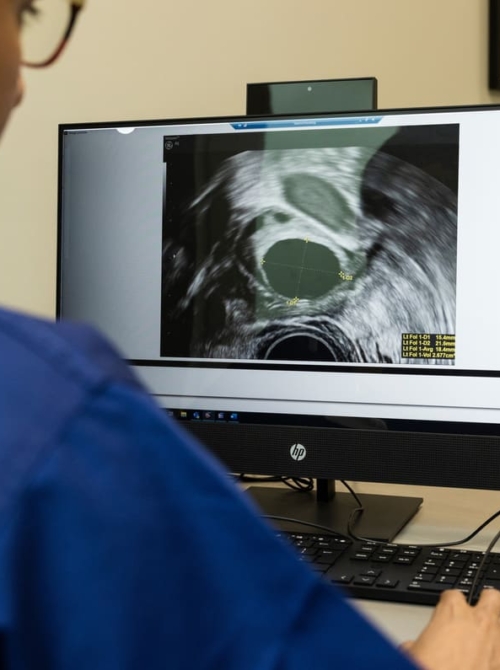
PCOS is a hormonal condition that can affect how and when you ovulate and is often linked to irregular or absent periods. You may also experience symptoms like acne, unwanted hair growth, or be told during an ultrasound that there are multiple small follicles on your ovaries. Because ovulation isn’t always predictable, getting pregnant with PCOS can sometimes take longer.
Endometriosis
Endometriosis happens when tissue similar to the lining of the womb grows outside the uterus, often around the ovaries, fallopian tubes, or other areas in the pelvis. This can cause inflammation, pain, and sometimes scar tissue, all of which may affect how easily an egg is released, fertilised, or implanted.
Not everyone with endometriosis has symptoms, but common signs include painful periods, pelvic pain throughout the cycle, fatigue, or digestive discomfort. And while it can impact fertility, many people with endometriosis do become pregnant – sometimes naturally, and sometimes with support.
PCOS vs endometriosis: key differences
| PCOS | Endometriosis | |
| Cause | Hormonal imbalance | Endometrial-like tissue outside the uterus |
| Ovulation | Often irregular or absent | Usually regular, but can be affected |
| Common symptoms | Irregular periods, acne, and excess hair | Painful periods, pelvic pain, fatigue |
| Fertility impact | Affects ovulation | Affects fertilisation and implantation |
| Diagnosis | Hormone tests, ultrasound | Ultrasound, laparoscopy |
Both conditions can be complex, and they affect everyone differently. But they are also manageable, and with early diagnosis and the proper fertility care, many people go on to have healthy pregnancies.
How do PCOS and endometriosis affect fertility?
Understanding how PCOS and endometriosis impact fertility can help make sense of why getting pregnant might be taking longer and why specific treatments are recommended.
PCOS and fertility: what’s going on?
In PCOS, the hormonal signals that control ovulation are often disrupted. Higher levels of androgens (male-type hormones) and insulin resistance can interfere with the growth and release of a mature egg. Without ovulation, there’s no egg available for fertilisation.
Even when ovulation does happen, it might not be predictable or consistent, making it harder to time conception. In some cases, the hormonal environment can also affect the quality of the egg or the development of the uterine lining, making implantation less likely.
Endometriosis and fertility: the underlying challenges
Endometriosis affects fertility in more complex ways. The condition creates inflammation in the pelvic cavity, damaging the environment where fertilisation and implantation occur.
This inflammation may impact how the sperm and egg interact in the fallopian tubes. Endometriosis can cause scar tissue or adhesions in more advanced cases, which may physically block or distort the reproductive organs.
Even when fertilisation occurs, endometriosis can affect the uterine lining in subtle ways, making it harder for an embryo to implant and grow.
What happens if you have both?
When PCOS and endometriosis occur together, they can affect different, but equally important, stages of the conception process.
- PCOS may make ovulation less likely
- Endometriosis may make fertilisation or implantation more difficult
This combination doesn’t mean pregnancy is out of reach, but it does mean a more detailed and personalised fertility assessment is often needed to understand where support is most effective.
Can you get pregnant with endometriosis or PCOS?
Many people with PCOS, endometriosis, or both conditions can and do get pregnant. But both conditions can affect how the body prepares for and supports conception. Factors like age, symptom severity, and how your body responds to treatment all play a role.
Trying to conceive with PCOS
Women with PCOS often respond well to ovulation-inducing medications, which help stimulate egg release. Others benefit from simple lifestyle adjustments, such as improving insulin sensitivity, managing stress, or improving sleep, which can help regulate hormone levels and restore ovulation.
If these approaches don’t lead to pregnancy, treatments like IVF are also highly effective, particularly in women with early diagnosis and good ovarian reserve.
Trying to conceive with endometriosis
Some people with mild or moderate endometriosis conceive naturally, especially if their cycles are regular and egg quality is unaffected. Others may benefit from keyhole surgery (laparoscopy) to remove endometriosis tissue, improving the chances of natural conception.
If conception doesn’t happen after a period of trying, IVF is often a recommended and successful option. It helps to bypass many of the physical barriers caused by endometriosis and can offer excellent success rates, particularly when treatment is tailored to your circumstances.
What if you have both?
When these conditions overlap, fertility can be affected by more than one factor. For example, PCOS may prevent regular ovulation, while endometriosis may impact egg quality, fertilisation or implantation. While this combination can complicate conception, many people still go on to have successful pregnancies with the right support.
Treatment plans are typically more tailored in this scenario. For some, a combination of ovulation induction and timed intercourse or IUI (intrauterine insemination) may be effective. Others may benefit from IVF, which allows specialists to optimise each stage of the conception process from egg development to embryo transfer.
PCOS and endometriosis fertility treatment options
When it comes to managing fertility with PCOS, endometriosis, or both, there isn’t a one-size-fits-all solution. Treatments depend on your symptoms, diagnosis, and fertility goals. Understanding the available options can help you feel more empowered and ready to discuss the best path forward with your specialist.
Treating PCOS-related fertility challenges
- Lifestyle adjustments
Many people with PCOS find that managing lifestyle factors like weight, diet, and exercise can help improve hormone balance and restore regular ovulation. Even a modest amount of weight loss can significantly improve insulin sensitivity and menstrual regularity. - Ovulation induction medications
If lifestyle changes aren’t enough, medications like letrozole or clomiphene citrate are commonly prescribed to stimulate ovulation. These drugs encourage the ovaries to release eggs regularly, improving the chance of natural conception or supporting timed intercourse and intrauterine insemination (IUI). - Metformin
In cases where insulin resistance is a concern, metformin may be used alongside ovulation induction to help regulate blood sugar and hormones. - IVF
When medications don’t lead to pregnancy, or if other factors are involved, IVF can be a highly effective next step. IVF bypasses many of the challenges caused by PCOS by controlling egg development and fertilisation in the lab.
Treating endometriosis-related fertility challenges
- Pain and symptom management
While symptom control alone doesn’t improve fertility, managing pain and inflammation can improve quality of life and overall well-being during treatment. - Surgical treatment
Laparoscopic surgery to remove endometriosis lesions and scar tissue can restore the pelvic environment and improve fertility, especially in moderate to severe cases. Surgery may be recommended before attempting conception or fertility treatment. - IVF
For many with endometriosis-related infertility, IVF may offer one of the most effective chances of pregnancy. IVF bypasses damaged fallopian tubes and the hostile pelvic environment, directly fertilising eggs and transferring healthy embryos to the uterus. - Other fertility treatments
In certain cases, treatments like IUI may be considered, particularly if endometriosis is mild and other fertility factors are favourable.
Treating PCOS and endometriosis
Managing fertility when both PCOS and endometriosis are involved requires a personalised and often multi-step approach. Treatment may involve a tailored combination of ovulation induction, surgery or assisted reproduction, depending on your circumstances.
Your fertility specialist will carefully assess which combination of treatments offers the best chance of success, supporting you every step of the way with expert guidance and compassionate care.
When to seek help
If you’re experiencing difficulties conceiving and have PCOS, endometriosis, or both, it’s important to know when to reach out for support. Early intervention can make a significant difference in understanding your unique situation and exploring the most effective treatment options.
You should consider seeking help if:
- You’ve been trying to conceive for 6 months or more and are over 35 years old
- You’ve been trying for 12 months or more and are under 35
- You’re experiencing painful, irregular, or absent periods that concern you
- You experience persistent pelvic pain or other symptoms that affect your well-being
- You have been diagnosed with PCOS, endometriosis, or both and want to understand how this might impact your fertility
At The Evewell, we offer compassionate, expert-led care tailored to your individual needs. Whether you’re just starting to explore your fertility or ready to take the next step, our dedicated team is here to support you every step of the way.
Book a consultation with The Evewell today and take the next step towards your fertility goals.
All Categories
Frequently asked questions
Yes, it’s absolutely possible to conceive naturally with PCOS and endometriosis. Many people go on to have successful pregnancies without fertility treatment, particularly when symptoms are mild or well managed.
Fertility declines gradually with age, for everyone, but people with PCOS and/or endometriosis may benefit from thinking about fertility earlier, particularly if symptoms are severe or cycles are irregular. Generally, fertility outcomes are better before the age of 35, but this isn’t a strict cut-off. Everyone’s situation is different, and personalised fertility testing can provide a clearer picture, whatever your age.
Yes, IVF can be an effective option for people who have both PCOS and endometriosis. It offers the benefit of bypassing ovulation difficulties (common in PCOS) and any physical barriers or inflammation affecting fertilisation or implantation (common in endometriosis). With careful hormonal management and expert care, IVF outcomes can be very positive, especially when treatment is tailored to your specific needs.
The best treatment depends on the severity of the endometriosis, your age, and how long you’ve been trying to conceive. For some, keyhole surgery (laparoscopy) to remove endometriosis tissue can improve natural conception rates. For others, IVF may offer the best chance of pregnancy, especially if the fallopian tubes are affected or previous surgery hasn’t led to success. Your fertility specialist will guide you through the most suitable options based on your unique case.
Yes, some people with endometriosis have no trouble conceiving, especially if the condition is mild and cycles are regular. Fertility outcomes vary widely from person to person, and not everyone with endometriosis will experience infertility. If you’re unsure how endometriosis might be affecting your fertility, a detailed assessment can offer clarity and peace of mind.