How age affects male fertility: what you need to know
When we talk about fertility and age, the conversation often centres around women. It’s well known that female fertility declines over time, especially after 35. But what’s less widely discussed, and frequently misunderstood, is that male fertility is also affected by age.
Here, Dr Nikolas Blontzos, Fertility Consultant at The Evewell West London, explores how male fertility changes over time, what factors play a role, and how men can take steps to protect and support their reproductive health at any stage of life.
What happens to male fertility with age?
Unlike women, who experience a more defined drop in fertility with menopause, the changes in male fertility tend to be slower and more subtle. This gradual shift can give the impression that time isn’t a major factor, but that’s not entirely accurate.
As men age, several aspects of sperm health, including movement (motility), shape (morphology), and genetic quality, begin to change. These shifts are often more prevalent after the age of 40 and can make it harder to conceive.
Hormonal changes
Testosterone plays a central role in male fertility, influencing everything from sperm production to libido. As men get older, natural testosterone levels may begin to fall. While this doesn’t stop fertility altogether, it can affect sexual function and reduce the efficiency of sperm production.
Sperm production slows
Men continue to produce sperm throughout life, but the process may become less effective over time. As the body ages, the number of healthy, motile sperm can begin to decline, particularly after age 40. This can delay conception, especially if other factors are also at play.
DNA ageing
Just like the rest of the body, sperm cells undergo ageing. Over time, exposure to oxidative stress and other biological processes can cause small breaks in sperm DNA. These changes don’t always prevent conception, but they may influence embryo development or increase the risk of complications.
Lifestyle and environmental factors
Over the years, lifestyle habits and environmental exposures can accumulate and influence reproductive health. Factors such as smoking, alcohol use, weight gain, poor diet, or exposure to environmental toxins can all impact sperm quality. While these habits aren’t exclusive to older men, their effects may become more pronounced with age.
_________
Male fertility age chart
A large-scale study, The Effect of Ageing on Semen Parameters, analysed semen samples across different age groups. The findings highlight how sperm characteristics of men change with age:
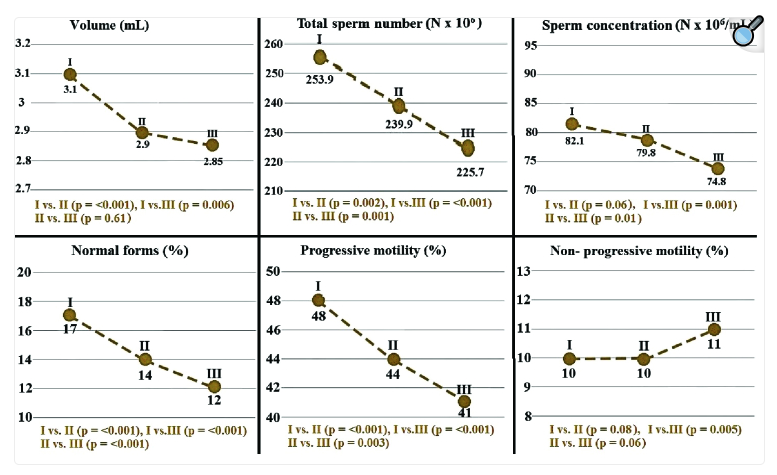
Semen parameter values among groups (I: Group I, age range: 18-29, n = 629, II: Group II, age range 30-39, n = 775, III: Group III, age range 40-49, n = 190). Source: The Effect of Ageing on Semen Parameters Study
Across these groups, researchers found a decline in average sperm count, motility, and morphology with age, emphasising that while conception is still possible in later years, it may take longer and come with increased risks.
_________
How age affects male fertility
Although male fertility doesn’t decline as sharply as it does in women, it’s not immune to the effects of time. Subtle shifts begin to occur – often gradually – and while they don’t always prevent conception, they can make it more difficult to conceive or influence the chances of a successful pregnancy.
Below, we look at some of the most common changes that may occur as men get older:
Sperm count and motility
One of the most noticeable changes is a reduction in sperm count – the number of sperm in a man’s semen. Additionally, sperm motility (how well sperm move) may also decrease. Since sperm need to swim efficiently to reach and fertilise the egg, reduced motility can lower the chances of conception.
Decreased sperm morphology
Morphology refers to the shape and structure of sperm. As men age, a higher percentage of sperm may have abnormalities in shape, which can make it harder for them to fertilise an egg. While some level of variation is normal, an increase in irregular morphology can impact fertility over time.
Lower seminal volume
Seminal volume, the total amount of fluid released during ejaculation, can also decrease with age. While this might not directly affect fertility on its own, lower volume can mean fewer sperm are delivered, which may reduce the chances of successful conception.
Sperm DNA damage
Ageing is also linked to an increased risk of sperm DNA fragmentation. This means the genetic material carried by sperm may become more prone to damage, which could influence embryo development and therefore affect the chances of a healthy pregnancy.
Erectile dysfunction
While not solely age-related, erectile dysfunction becomes more common as men get older. This can sometimes be caused by lower testosterone levels or health conditions that develop with age, such as cardiovascular issues or diabetes. In some cases, erectile dysfunction can affect the ability to conceive by reducing the frequency or success of intercourse.
Taken together, these changes may not cause infertility outright, but they can make it more difficult to achieve a pregnancy.
_________
Male fertility age and pregnancy outcomes
Whilst it’s possible to conceive healthy children later in life – and many men do – studies suggest that increased paternal age may be linked to certain risks during conception and pregnancy.
For example, miscarriage risk may rise with older paternal age, even when the female partner is younger. This is thought to be due to higher rates of DNA fragmentation in sperm.
There’s also some evidence of a small increase in the likelihood of birth defects or conditions like autism or schizophrenia in children born to older fathers. These risks remain low in absolute terms, but they do increase slightly after the mid-40s.
_________
Supporting male fertility with positive lifestyle choices
While age is something no one can control, positive lifestyle choices are one area that can make a real impact. The following steps can help protect and support male fertility:
- Diet: A nutrient-rich, balanced diet supports sperm quality and hormone health.
- Alcohol: Reducing alcohol can improve testosterone levels and sperm production.
- Stop Smoking: Smoking is linked to poor sperm health and higher DNA damage.
- Exercise: Regular, moderate activity helps balance hormones and reduces stress.
- Sleep: Good-quality sleep helps regulate testosterone levels and supports overall fertility.
- Stress Management: Chronic stress can disrupt reproductive hormone levels.
- Supplements: Antioxidants such as zinc, selenium, and CoQ10 may improve sperm health.
By making supportive lifestyle changes early, men can help preserve their fertility potential and improve their chances of successful conception.
Find out more in our ‘How to increase fertility in men’ article.
_________
Treatments for age-related male infertility
While age-related changes in fertility can’t be reversed, some effective treatments and technologies can help support men in their fertility journey. At The Evewell, we offer tailored guidance to help identify the most appropriate path forward based on each person’s individual circumstances.
If age-related changes have affected sperm quality or quantity, assisted reproductive techniques can help increase the chances of conception.
- Intrauterine Insemination (IUI): IUI involves placing specially prepared sperm directly into the uterus around the time of ovulation. This method can be helpful for men with slightly reduced sperm motility or count, as it brings sperm closer to the egg at the optimal moment.
- Intracytoplasmic Sperm Injection (ICSI): ICSI is a specialised form of IVF, where a single healthy sperm is injected directly into an egg. It’s often recommended in cases of low sperm count, poor motility, or previous failed fertilisation, and can improve the chances of success when sperm quality is affected by age.
- In Vitro Fertilisation (IVF): IVF is often recommended when fertility issues are more significant or when multiple factors are involved. It involves collecting eggs and sperm, then fertilising them in a lab before transferring the best-quality embryo back into the womb. IVF can bypass many of the natural barriers that may prevent conception.
Sperm freezing
If you’re not ready to start a family now, but want to preserve fertility for the future, sperm freezing is a valuable option. It’s also recommended ahead of medical treatments, such as chemotherapy, that could affect fertility. By freezing sperm at a time when quality is at its best, men can help protect their future options, whether for use in IUI, IVF, or other fertility treatments later on.
_________
Male fertility testing
If pregnancy isn’t happening as expected, or if you simply want to understand more about your reproductive health, a male fertility test can offer valuable insight.
Testing typically involves a semen analysis that assesses key indicators such as sperm count, motility, morphology (shape), and volume. In some cases, additional tests may be recommended, such as hormone checks or DNA fragmentation testing, to give a fuller picture of fertility potential.
At The Evewell, we offer discreet, specialist-led fertility assessments for men, designed to be as informative and reassuring as possible. Whether you’re trying to conceive now or planning for the future, we’re here to help guide the next steps with clarity and care.
All Categories
Discover more
Find out more
Frequently asked questions
Male fertility tends to be at its peak in the late teens to early 30s. During this time, sperm count, motility, and overall quality are typically at their highest. While men can still conceive later in life, sperm health can gradually decline with age, particularly after 35.
Sperm count is a key factor in male fertility. According to the World Health Organisation (WHO), a normal sperm count is 15 million sperm per millilitre or more. That said, fertility is about more than just numbers; factors like sperm motility (how they swim) and morphology (how they’re shaped) also matter. Even with lower counts, natural conception is still possible, especially when other aspects of reproductive health are in good shape.
There’s no exact age when male fertility stops – unlike female fertility, which is limited by menopause. Men can technically father children into their 50s, 60s and beyond. However, the chances of conception may decrease, and there may be a slightly higher risk of complications due to changes in sperm quality over time.
Fertility declines gradually, rather than suddenly. After 35, studies show that sperm motility and morphology tend to decrease, and DNA fragmentation may increase. This can lower the chances of conception and may slightly increase the time it takes to conceive, particularly when combined with other factors.
Fertility often doesn’t cause noticeable symptoms, but good general health, regular sexual function, and no known medical concerns can be reassuring signs. The only way to know for certain is through a semen analysis, which looks at sperm count, shape, movement, and volume.
The most accurate way to check male fertility is with a semen analysis. This simple test measures key factors like sperm count, motility, and morphology. At The Evewell, we offer discreet, expert-led testing alongside supportive guidance, so individuals and couples can plan with confidence.





